All of our recommendations, unless specified, relate to acute COVID-19 in adults.
Some of our recommendations vary according to the severity of COVID-19 illness. Definitions of the categories are based on World Health Organization (WHO) criteria and can be viewed by clicking the plus (+) signs below.
Definition:
NO features of severe or critical illness (see below). For some interventions this group may be divided into:
Mild illness
- Symptomatic (any acute COVID-19 related symptoms)
- AND respiratory rate <24/min
- WITHOUT pneumonia or hypoxia
Moderate illness
- Pneumonia (clinical or radiological) OR hypoxia (SpO2 <94% in adults with no underlying lung disease)
- AND respiratory rate ≤30/min
- AND SpO2 ≥90% on room air
- AND no respiratory distress
Definition:
Pneumonia with ANY ONE of the following:
- respiratory rate >30/min
- severe respiratory distress
- SpO2 <90% on room air
- NO invasive or non-invasive respiratory support needed
Definition:
- Requirement for high-level respiratory support: noninvasive ventilation, high-flow oxygen (≥20 litres per minute) or invasive mechanical ventilation
- OR acute respiratory distress syndrome (PaO2/FiO2 ratio of <300)
- OR sepsis
- OR shock
Recommendation: We recommend against using Ivermectin for treatment of patients with any severity of COVID-19, except in the context of a clinical trial.
Date of recommendation: XX/XX/XXXX
Ivermectin has been shown to inhibit the replication of SARS CoV2 in vitro. Ivermectin binds and destabilises the viral protein and prevents it from entering the nucleus. However, the drug dosages used in these in vitro studies far exceed those that have been used for other conditions. Drug doses and levels required to achieve therapeutic effects in vivo based on these studies probably exceed the safety margins.
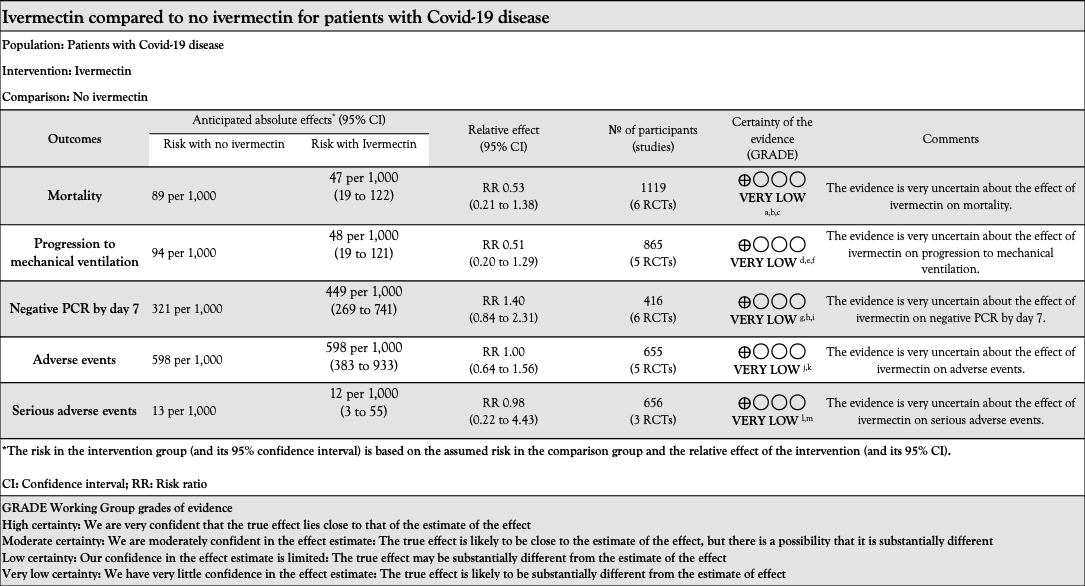
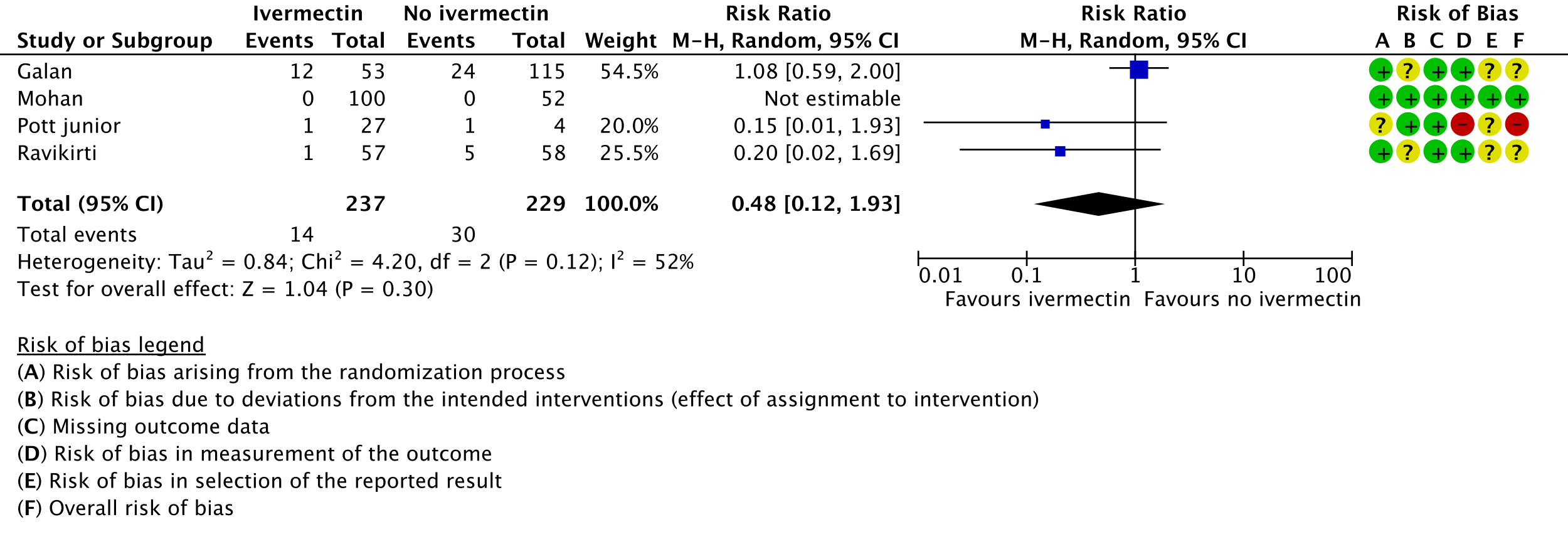
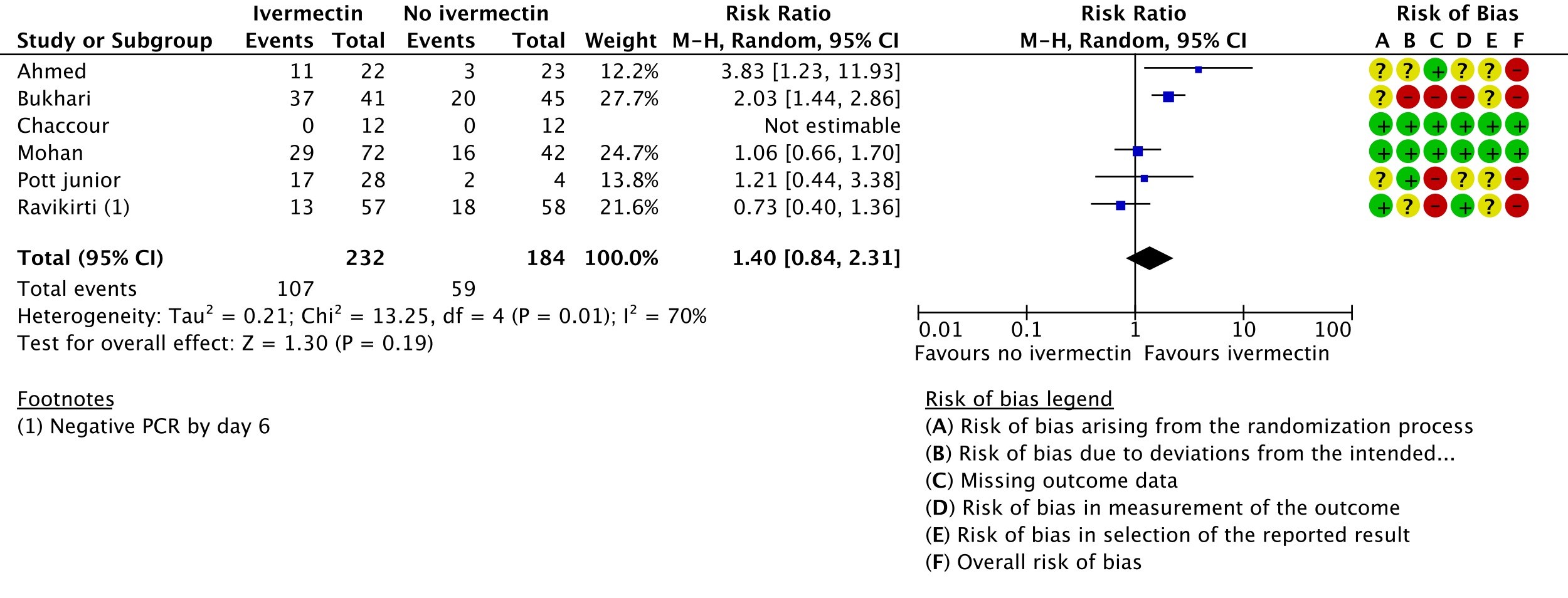
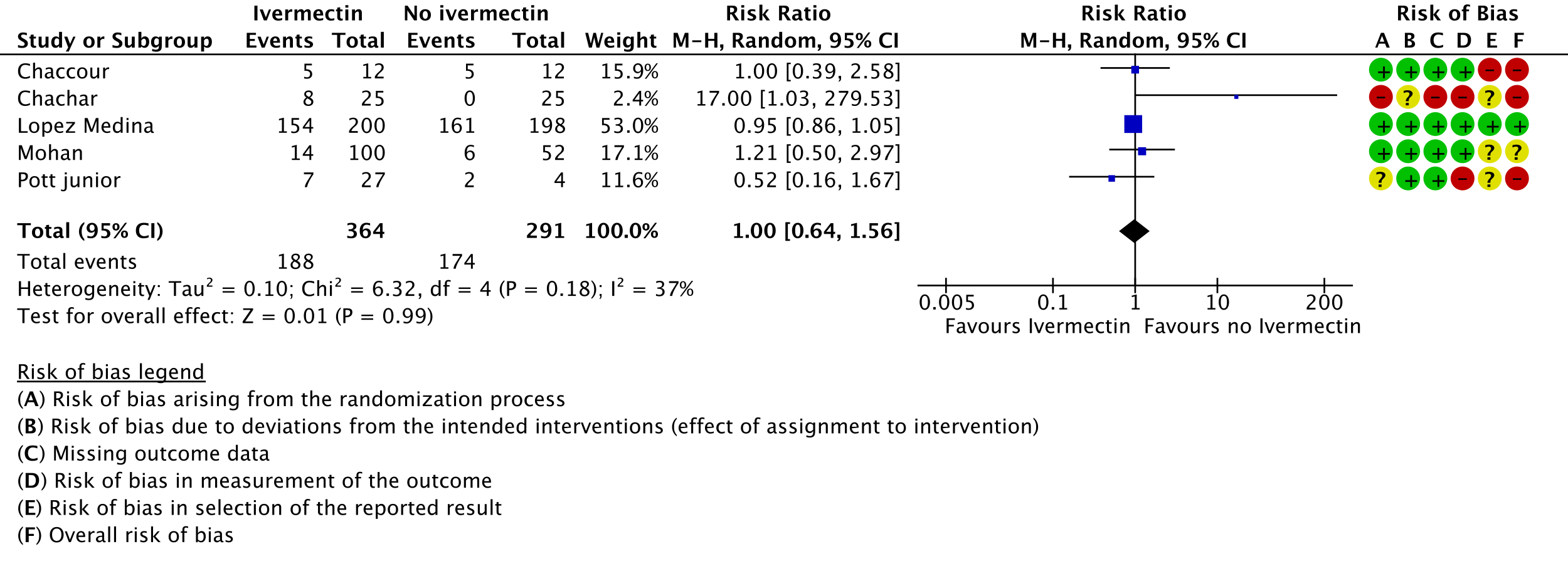
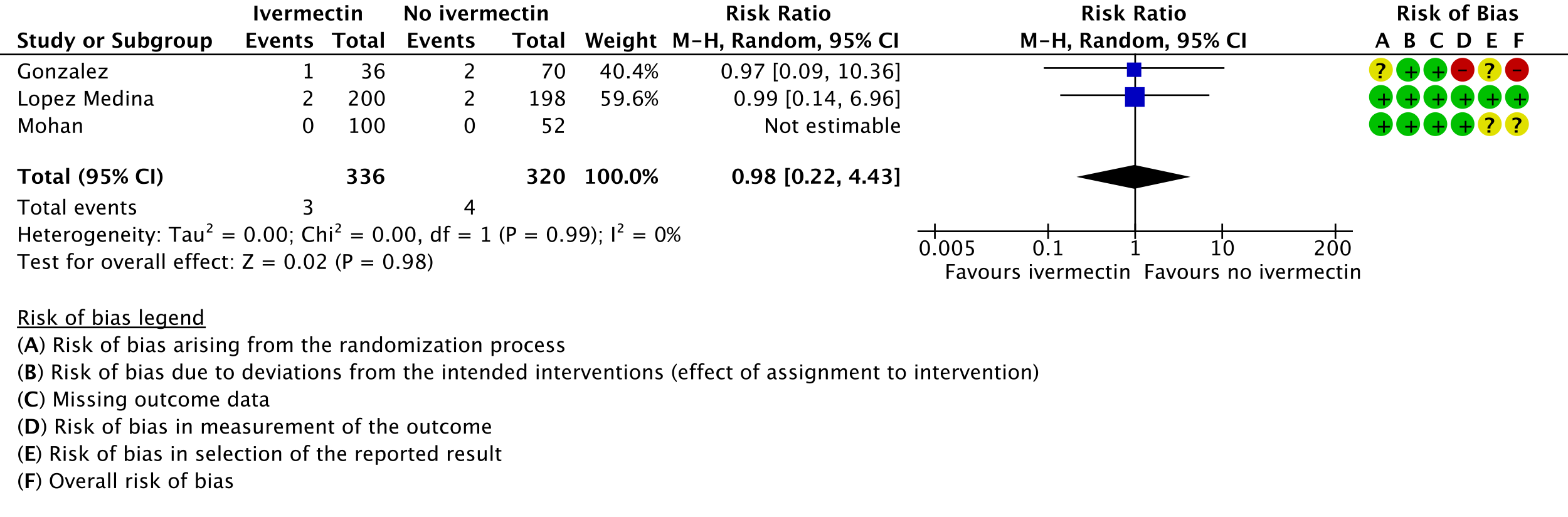
The trials since published have used varying doses and approaches to outcome measurement and reporting, and have varying degrees of bias reported in various domains of the Cochrane ROB2 tool. Due to inconsistency, imprecision and risk of bias of the effect estimates, the evidence is very uncertain about the effect of Ivermectin in preventing mortality, progression to mechanical ventilation, time to a negative PCR by day 7 and serious or all adverse effects.
Thus at this time we would recommend against using Ivermectin except in the context of a clinical trial, as it would distract from conduct of good trials which could address this lacuna, or for an individual patient distract from use of other efficacious management interventions. Indiscriminate use of this drug will possibly also have repercussions on availability of its use in conditions where its use is definitely indicated i.e. in parasitic infections.
Ivermectin is widely available, relatively inexpensive and has low risk of adverse drug reactions and may be used citing that lack of evidence of benefit is not evidence of lack of benefit. However, there are likely indirect harms. Its use may lead to a false sense of security. This could hamper close monitoring, and cause delay in the use of other interventions for which better evidence of benefit exists and have to be used in a suitable time frame.
This recommendation is based on the evidence to date, and will be updated as new evidence emerges. If ivermectin is subsequently assessed to be effective and safe in the treatment of COVID-19, it should be relatively feasible to implement this in management protocols.
Lack of uniform criteria for COVID-19 severity, substantial overlap and lack of clear reporting of severity in the included trials prevented a meaningful subgroup analysis by severity.
Furthermore, a lack of within trial comparison prevented subgroup analysis by age, duration of symptoms or dose of ivermectin. In addition, data of safety and efficacy in specific subgroups such as pregnancy, children, liver and kidney disease were not available in the trials included in the rapid review.
This conditional recommendation against use of ivermectin will be revisited as evidence emerges. In addition to evidence of benefit, with its widespread use in India, there may be additional real-world reports regarding undesirable effects, which the group will monitor. Although ivermectin is generally well tolerated, adverse effects like dizziness, tachycardia, postural hypotension diarrhoea, arthralgia, and facial and peripheral oedema have been reported even with single doses as used in parasitic diseases. Encephalopathy with permanent disability has been reported when ivermectin has been used in the treatment of onchocerciasis or other parasitic diseases. It is predominantly metabolized in the liver (CYP3A4), which may lead to drug-drug interactions.
Ivermectin has been used in varying doses and duration in the trials included in the present review. Though absolute event numbers suggest that the incidence of adverse effects was not higher in those receiving ivermectin, there is very low certainty in the evidence. Hence this precludes confidence that there is indeed no expected increase in serious adverse effects.
Further evidence for the use of Ivermectin in the treatment of COVID-19 needs to be generated from well-conducted randomized double-blind placebo-controlled trials which are adequately powered and have a low risk of bias. These should be designed to study the effect of Ivermectin on critical and important clinical outcomes as well as adverse effects. Utility in pre-specified patient sub-groups like mild, moderate, or severe infection, special populations (immunosuppressed, pregnant, children, comorbid conditions), and various phases of the illness will also need to be addressed.
However, given the unlikely biological plausibility of attaining effective in vivo SARS-CoV-2 inhibitory concentrations at the currently labelled dose range, Ivermectin as an antiviral may not be effective. There are reports that though higher doses do cause adverse effects, they are unlikely to result in any life-threatening complications. However this uncertainty needs to be evaluated longitudinally in a systematic manner. Furthermore, emergence of new data suggesting a role in modulation of the potential immune response in COVID 19 need to be explored.
Evidence synthesis team: Harshdeep Acharya, Audrin Lenin, Richard Kirubakaran, Priscilla Rupali and Bhagteshwar Singh
Valuable assistance with performing the evidence synthesis was provided by the author team of an ongoing Cochrane systematic review: Popp M, Stegemann M, Metzendorf M-I, Kranke P, Meybohm P, Skoetz N, Weibel S. Ivermectin for preventing and treating COVID‐19. Cochrane Database of Systematic Reviews 2021, Issue 4. Art. No.: CD015017. DOI: https://doi.org/10.1002/14651858.CD015017.
Explanations:
a. Downgraded by 1 level for serious risk of bias. Due to Niaee and Galan having High risk of bias (2 out of 6). 2 other trials Gonzalez and Ravikirti had some concerns for risk of bias.
b. Downgraded by 1 level for serious inconsistency. Due to substantial heterogeneity (I2=62%) and visually some trials having point estimates very far from others.
c. Downgraded by 2 levels for very serious imprecision. Due to small absolute number of events, CIs overlapping no effect and inability to exclude serious benefit or serious harm.
d. Downgraded by 1 level for serious risk of bias. Due to Pott-Junior having High risk of bias (1 out of 4). 2 other trials Galan and Ravikirti had some concerns for risk of bias.
e. Downgraded by 1 level for serious inconsistency. Due to substantial heterogeneity (I2=48%) and visually some trials having point estimates very far from others.
f. Downgraded by 2 levels for very serious imprecision. Due to small absolute number of events, CIs overlapping no effect and inability to exclude serious benefit or serious harm.
g. Downgraded by 2 levels for very serious risk of bias. Due to Bukhari, Ahmed and Pott-Junior having high risk of bias for this outcome, this limits our confidence in the results.
h. Downgraded by 1 level for serious inconsistency. Due to substantial heterogeneity (I2=70%) and visually some trials having point estimates very far from others.
i. Downgraded by 1 level for serious imprecision. Due to CIs overlapping no effect and inability to exclude important benefit.
j. Downgraded by 1 level for serious risk of bias. Due to Chachar, Chaccour and Pott-Junior having High risk of bias (3 out of 5). Lopez-Medina which carries 53% weight in the forest plot is low risk of bias.
k. Downgraded by 2 levels for very serious imprecision. Due to CIs overlapping no effect and inability to exclude important benefit and important harm.
l. Downgraded by 1 level for serious risk of bias. Due to Gonzalez having High risk of bias (1 out of 3).
m. Downgraded by 2 levels for very serious imprecision. Due to CIs overlapping no effect and inability to exclude important benefit and important harm.
The use of ivermectin for treatment of COVID-19 started after reports of the drug showing reduction in viral load of SARS-CoV-2 in in vitro studies (1). However, due to lack of conclusive evidence, World Health Organization recommends use of ivermectin only in clinical trials (2). Use continues widely, including self-medication, especially in low- and middle-income countries due to easy availability and low cost of the drug (3). This review aims to provide a summary of the available evidence from randomised clinical trials of ivermectin for treatment of acute COVID-19, for any dose or duration, which could guide clinicians and researchers regarding the appropriate use of this drug in the future.
We used Cochrane rapid review methodology. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Epistemonikos, and the COVID‐19‐specific resource www.covid‐nma.com, for studies of any publication status and in any language. We also reviewed reference lists of systematic reviews and included studies. We performed all searches up to 15 April 2021. We contacted researchers to identify unpublished and ongoing studies.
We included randomized controlled trials (RCTs) testing ivermectin in people with COVID‐19, and planned to extract data for the following pre-defined outcomes:
- Critical (primary for this review):
- Mortality (all-cause) – at 28-30 days, or in-hospital
- Progression to:
- Oxygen therapy
- Ventilation: non-invasive or invasive
- Critical or Intensive care (any reason) - Duration of hospitalization
- Need for hospitalization (for out-patients)
- Adverse events: all and serious
- Important (secondary):
- Time to clinical improvement
- Time to negative PCR for SARS-CoV-2
- Negative PCR for SARS-CoV-2 by day 7 post-enrolment
- Complications of COVID-19:
- Thrombotic events
- Pulmonary function/fibrosis
- Long covid/post acute sequelae COVID
- Secondary infections
Two reviewers independently assessed eligibility of search results. One reviewer extracted data from each included study, and assessed risk of bias using the Cochrane Risk of bias (RoB) v2.0 tool. Data and RoB assessments were checked against a Cochrane systematic review team’s extractions and assessments (who used a consensus approach). In case of any discrepancies, the whole RoB assessment was scrutinised by the whole team for this review, to reach consensus. We used risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs). We performed meta‐analysis using a random‐effects model for outcomes where pooling of effect estimates was appropriate.
We included 12 trials involving 1413 participants, all of whom were adults, and 718 of whom received ivermectin (4-15). There were two trials each from Brazil, India and Pakistan; one trial reported from each of Bangladesh, Colombia, Iran, Mexico, Nigeria, and Spain. Eight were in hospitalized patients, one recruited outpatients only, one recruited both, and two did not report care setting. Disease severity, prevalence of comorbidities, and use of co‐interventions varied substantially between trials. We found potential risks of bias across all domains; 10 of the 12 trials were at high risk of bias overall for at least one outcome. Risk of bias for each domain per trial is displayed alongside the Forest plots below.
The following comparisons were investigated in the trials (we compared outcomes for arms randomised to ivermectin vs. outcomes for arms randomised to anything else):
- Six trials compared ivermectin with placebo (793 participants)
- Two compared ivermectin with standard care (212 participants)
- One compared ivermectin vs. placebo vs. a combination of ivermectin & doxycyline in three arms (72 participants; 24 participants in ivermectin & doxycycline arm excluded)
- One compared ivermectin vs. placebo vs. hydroxychloroquine in three arms (106 participants)
- One compared ivermectin with lopinavir/ritonavir (62 participants)
- One compared ivermectin with chloroquine or hydroxychloroquine (168 participants)
As presented in the ‘Summary of findings’ table, the evidence is very uncertain about the effect of ivermectin on mortality; progression to mechanical ventilation; negative PCR for SARS-CoV-2 by day 7; adverse events; and serious adverse events. For mortality, there were no significant differences observed when trials were stratified by COVID-19 illness severity or risk of bias.
One trial reported a higher risk of discontinuation of ivermectin vs. placebo due to an adverse event (RR 2.97; 95% CI 1.10 to 8.02; 1 trial; 398 participants).
Pooled effect estimates for all of the following outcomes not included in the summary of findings table had 95% confidence intervals which included potential benefit and potential harm from ivermectin: need for critical or intensive care (2 trials; 283 participants); discharge from hospital by day 10 post-enrolment (1 trial; 115 participants); time to clinical improvement (4 trials; 211 participants); deterioration by 2 points on 8-point clinical ordinal scale (1 trial; 398 participants); lack of fever on day 7 (1 trial; 36 participants); lack of symptoms on day 7 (1 trial; 50 participants); negative PCR for SARS-CoV-2 on day 10 (1 trial; 62 participants); and thrombotic events (1 trial; 106 participants).
No comparative data could be extracted for risk of progression to oxygen therapy; need for hospitalisation in outpatients; or post-acute COVID-19 pulmonary function/fibrosis or other sequelae; or secondary infections.
1. Mortality, stratified by risk of bias: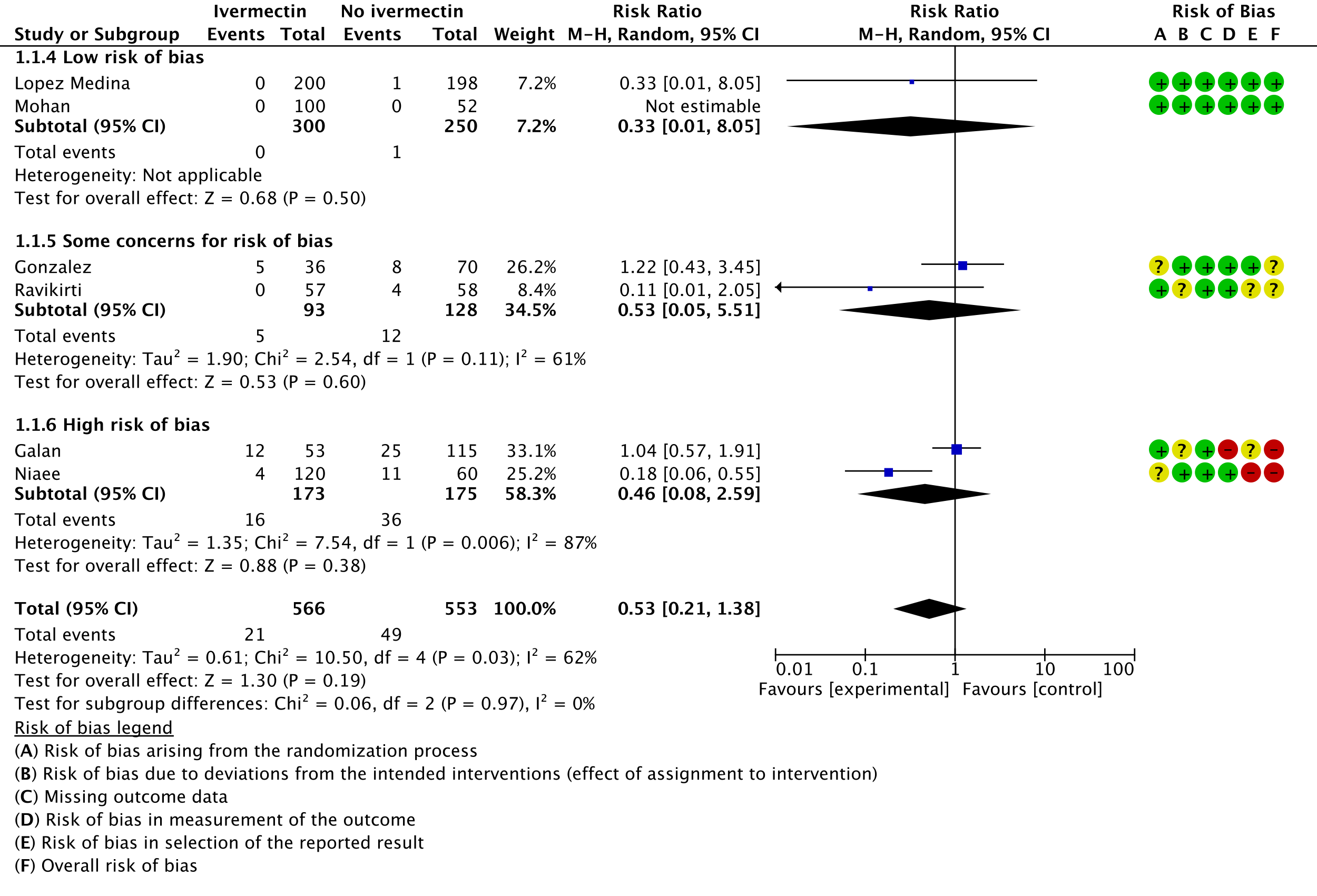
2. Progression to mechanical ventilation:
3. Negative PCR for SARS-CoV-2 by day 7:
4. Adverse events:
5. Serious adverse events:
- Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020 Jun;178:104787.
- Therapeutics and COVID-19: living guideline [Internet]. [cited 2021 Apr 26]. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-therapeutics-2021.1
- Molento MB. COVID-19 and the rush for self-medication and self-dosing with ivermectin: A word of caution. One Health. 2020 Dec;10:100148.
- Ahmed S, Karim MM, Ross AG, et al. A five-day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Dis. 2021 Feb;103:214-216. https://doi.org/10.1016/j.ijid.2020.11.191.
- Babalola OE, Bode O, Ajayi AA, et al. Ivermectin shows clinical benefits in mild to moderate COVID19: A randomised controlled double-blind, dose-response study in Lagos. QJM: An International Journal of Medicine, 2021;hcab035. https://doi.org/10.1093/qjmed/hcab035.
- Bukhari KHS, Asghar A, Perveen N, et al. Efficacy of ivermectin in COVID-19 patients with mild to moderate disease. medRxiv [preprint]. 2021.02.02.21250840; https://doi.org/10.1101/2021.02.02.21250840.
- Chaccour C, Casellas A, Blanco-Di Matteo A, et al. The effect of early treatment with ivermectin on viral load, symptoms and humoral response in patients with non-severe COVID-19: A pilot, double-blind, placebo-controlled, randomized clinical trial. EClinicalMedicine. 2021 Feb;32:100720. https://doi.org/10.1016/j.eclinm.2020.100720.
- Chachar AZK, Khan KA, Asif M, et al. Effectiveness of ivermectin in SARS-CoV-2/COVID-19 patients. International Journal of Sciences. 09(2020):31-35. https://doi.org/10.18483/ijSci.2378.
- Galan LEB, Santos NMD, Asato MS, et al. Phase 2 randomized study on chloroquine, hydroxychloroquine or ivermectin in hospitalized patients with severe manifestations of SARS-CoV-2 infection. Pathog Glob Health. 2021 Mar 8:1-8. https://doi.org/10.1080/20477724.2021.1890887.
- Gonzalez JLB, Gámez MG, Enciso EAM, et al. Efficacy and safety of Ivermectin and Hydroxychloroquine in patients with severe COVID-19. A randomized controlled trial. medRxiv [preprint]. 2021.02.18.21252037. https://doi.org/10.1101/2021.02.18.21252037.
- López-Medina E, López P, Hurtado IC, et al. Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: A randomized clinical trial. JAMA. 2021 Apr 13;325(14):1426-1435. https://doi.org/10.1001/jama.2021.3071.
- Mohan A, Tiwari P, Suri T, et al. Ivermectin in mild and moderate COVID-19 (RIVET-COV): a randomized, placebo-controlled trial. Research Square [preprint]. https://doi.org/10.21203/rs.3.rs-191648/v1.
- Niaee MS, Gheibi N, Namdar P, et al. Ivermectin as an adjunct treatment for hospitalized adult COVID-19 patients: A randomized multi-center clinical trial. Research Square [preprint]. https://doi.org/10.21203/rs.3.rs-109670/v1.
- Pott-Junior H, Bastos Paoliello MM, Miguel AQC, et al. Use of ivermectin in the treatment of Covid-19: A pilot trial. Toxicol Rep. 2021;8:505-510. https://doi.org/10.1016/j.toxrep.2021.03.003.
- Ravikirti, Roy R, Pattadar C, et al. Ivermectin as a potential treatment for mild to moderate COVID-19 – A double blind randomized placebo-controlled trial. medRxiv [preprint]. 2021.01.05.21249310. https://doi.org/10.1101/2021.01.05.21249310.
The Antiviral Expert Working Group met on 28th April 2021 to consider ivermectin as a treatment for COVID-19. Conflict of interest declarations were reviewed by the Steering Committee; none were found to be relevant to ivermectin.
A summary and then more detailed explanations of the Expert Working Group's judgements follow.
Summary of judgements
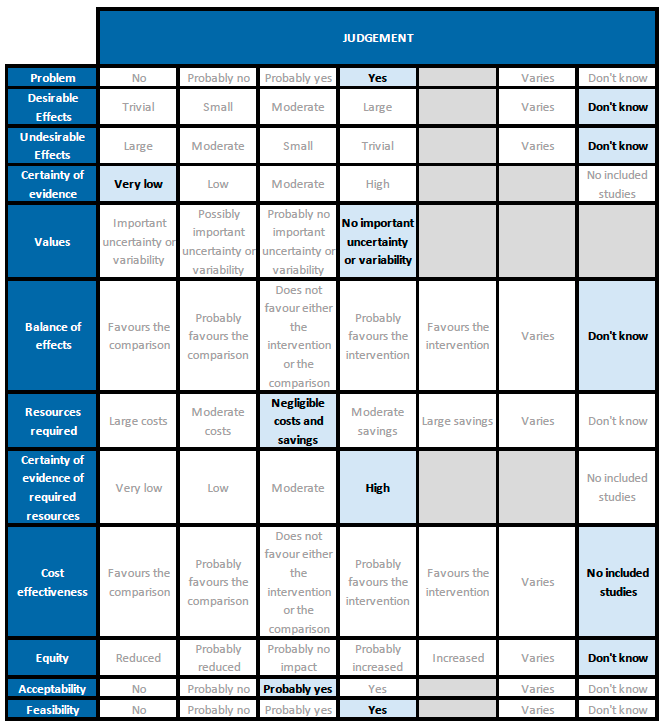
Problem
There is some evidence in the literature regarding use of ivermectin for treatment of COVID-19, but reports of trials and reviews are conflicting. Given current demand for effective treatments, the evidence needs to be examined, and a recommendation based on this would be a priority. The PICO question now applies for all patients with COVID-19 (initial PICO was for hospitalised patients).
Desirable effects
All 95% confidence intervals cross 1, for mortality, progression to ventilation and negative PCR at day 7. So we don't know if there is a difference. Pharmacokinetic modelling suggests that the dose of ivermectin used would not achieve high enough concentrations in vivo to kill SARS-CoV-2 in blood (but not necessarily in lung tissue). There have been some suggestions regarding potential immunomodulatory effect.
One trial reviewed by the evidence summary team mixed alcohol with ivermectin to increase bioavailability, based on pharmacokinetic modelling.
Undesirable effects
All 95% CIs cross 1, for adverse events and serious adverse events. This drug has been widely used and adverse effects at the dose used have not been reported commonly. Drug-drug interactions are possible, and use with dexamethasone may reduce ivermectin concentrations further.
One panel member reported ivermectin can also increase concentration of warfarin and a case of severe bleeding as a result of this.
There is also the indirect risk of harm from relying on this treatment and not using treatments with better evidence, such as good supportive care.
Certainty of evidence
Using GRADE methodology the team rated the certainty in the evidence as very low for all outcomes to which GRADE was applied. The panel agreed.
Values
The review included critical and important outcomes. Results were not reported for all, but results were found for four critical outcomes and one important outcome including death and adverse events.
Balance of effects
Very low certainty in the desirable or undesirable effects of ivermectin, with 'don't know' judgements. This means we do not know if ivermectin has an overall desirable vs. undesirable effect.
Ivermectin is part of the current Ministry of Health & Family Welfare protocol, for mild COVID-19 disease. Some reviews of the evidence have suggested a large beneficial effect, but the current review does not reflect this. Trials at higher risk of bias were the ones that reported a benefit. They include one trial excluded in this review as it was not a randomized trial on further inspection. The panel discussed whether an intervention should be given if there is no observed benefit, as there is a risk to giving any intervention (as in the Additional Considerations for Undesirable Effects section above).
Resources required
Cost of a dose, or a course as used in trials (up to 7 days of usual daily dose of up to 12mg) is low.
Certainty of evidence of required resources
Ivermectin is a low-cost treatment widely used in low- and middle-income settings for other conditions. Published evidence was not consulted for this judgement, as it has been used extensively by the expert working group for other conditions.
Cost effectiveness
None of the included trials assessed cost-effectiveness.
Equity
There is not enough information to make this judgement.
Acceptability
The panel noted that ivermectin is an oral drug, easy to administer, low cost, and relatively safe for other conditions. However, note the concerns raised in the Undesirable Effects section above. The panel felt that most patients, if they knew there was no evidence for benefit, would be unlikely to accept the drug.
Feasibility
Evidence was not specifically examined for COVID-19, but the panel is aware of reports of mass-drug administration of ivermectin in some countries.
The panel noted that this would be feasible to administer if found effective, however, we do not have data right now to suggest this. The panel felt a recommendation for use would only detract from other interventions which have reported an unequivocal benefit.
